Researchers investigate how a stressed brain can make asthma worse
Researchers at the University of Wisconsin-Madison are investigating cross-talk between the brain and lungs of people with asthma during a 4-year, $2.5 million study to understand how psychological stress can make asthma worse.
The effort is being conducted by members of two groups with international reputations: a team led by William Busse, MD (pictured below), professor, Asthma, Pulmonary and Critical Care Medicine, and another led by Richard Davidson, PhD, William James & Vilas Professor of Psychology & Psychiatry, thus bringing together the research world of asthma and the mind and achieving a longstanding need.
Dr. Davidson directs the UW-Madison Center for Healthy Minds, which is dedicated to cultivating well-being and relieving suffering through a scientific understanding of the mind.
The researchers hope to find ways to alter brain-lung communication, and thereby help manage asthma. Their clinical study is called AsthMatic Inflammation and Neurocircuitry Activation, or MINA.
A Project Twenty Years in the Making
The current investigation is a culmination of efforts by Dr. Busse and colleagues more than 22 years ago. He and other investigators specializing in asthma had long noticed connections between the level of day-to-day stresses faced by patients living with asthma, and how their disease was affected by these events.
"Depression and anxiety is a common finding among patients with asthma — up to 20 percent," said Dr. Busse, who had long noticed that patients with asthma who were also depressed, agitated, or faced other mental health challenges were more likely to be less responsive to treatment. "These are the ones who do not do well with their disease," he said.
While the pulmonary symptoms of asthma can be striking - wheezing, shortness of breath, and acute attacks called exacerbation, and can be deadly if not managed properly - the fact that asthma and its underlying airway inflammation are driven by immunological processes is not always recognized or appreciated.
And there is tantalizing evidence that the function of the immune system is linked to the function of the mind.
Mind Over Matter?
In the 1970s, research on rats by University of Rochester professor Robert Ader, PhD, showed that immunosuppression could be induced by first training rats to associate a sensation such as a sweet taste with a drug called cytoxan that depresses the immune system and leads to fatal infections.
Eventually, Dr. Ader found that feeding the rats a sweet solution alone in absence of the drug also caused them to become immunosuppressed, fall ill to viral and bacterial infection, and die.
Observations from the experiments led Dr. Adler to found the field of psychoneuroimmunology, which combines three disciplines: psychology, neurology, and immunology.
 Psychoneuroimmunology was a unique melding of approaches and ideas. From Dr. Busse's perspective, in the 1990s, the asthma research community was having difficulty in developing experimental methods that could pinpoint exactly how the mind could affect the immune system - and vice versa - in asthma and make the disease more severe.
Psychoneuroimmunology was a unique melding of approaches and ideas. From Dr. Busse's perspective, in the 1990s, the asthma research community was having difficulty in developing experimental methods that could pinpoint exactly how the mind could affect the immune system - and vice versa - in asthma and make the disease more severe.
The National Institutes of Health and the Fetzer Institute conducted a workshop on stress and asthma in Kalamazoo, Michigan on September 27-28, 1995. Both Dr. Busse and Dr. Davidson attended, as well as Chris Coe, PhD, professor, Department of Psychology. Dr. Coe and Dr. Busse had collaborated on early studies, including one investigating how students' stress from final exams affected asthma.
In a summary of this workshop, Dr. Busse wrote, "Stress may also alter susceptibility to infectious illness, particularly respiratory illness, as well as morbidity and mortality following infection. These and several related lines of research suggested novel avenues through which these central nervous system-neuroendocrine-immune system interactions could affect asthma." Attendees developed recommendations of animal and human studies that they felt should be prioritized to evaluate these possibilities.
Afterwards, Dr. Davidson (pictured at right talking with His Holiness the 14th Dalai Lama of Tibet in 2010) began talking with Dr. Busse about using the Davidson group's expertise in brain imaging techniques and psychological diseases in relation to asthma.
"The Fetzer Institute funded a pilot study. This was the first time we did imaging of the brain in relationship to an experimental provocation of asthma," said Dr. Busse. “More importantly, our efforts brought together two areas of research not commonly linked – asthma and the brain.”
“The fact that psychosocial stress can provoke an exacerbation of asthma symptoms clearly indicates that the brain must be involved since it is the brain that transduces stressful events into biological signals that ultimately influence lung function,” said Dr. Davidson. Precisely how this signaling occurs between the brain and the lung is the focus of their current collaborative work.
In time, a member of Dr. Davidson's laboratory dedicated herself to studying the neural-immune link and biochemical mechanisms underlying resilience or vulnerability to disease.
After finishing her undergraduate degree, Melissa Rosenkranz (pictured in the video below) took a position in the Davidson group to study the impact of meditation on the immune system.
She earned her PhD in his laboratory and today is an Associate Scientist at the Center for Healthy Minds.
"Working across disciplines is how my brain works. I would feel very bored and narrow-minded if I restricted myself to one of those disciplines," said Dr. Rosenkranz.
Chasing Down Pathways for Brain-Lung Signaling
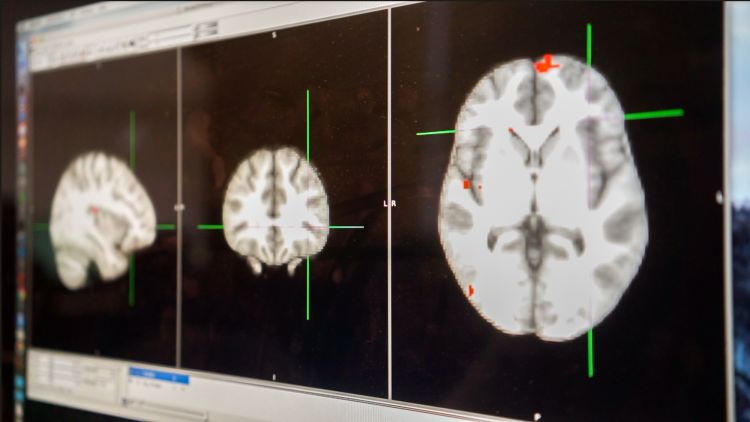
The collaboration between Dr. Busse, Dr. Davidson, and Dr. Rosenkranz led to three research studies. In 2005, the team published the results of specialized brain scans called functional magnetic resonance imaging (fMRI) on volunteers with asthma after they were exposed to allergen. They found that areas of the brain were activated in response to the allergic reaction in the lung. These findings were extremely novel and exciting, as they pointed to potential pathways between asthma and the brain.
They extended this work in a study published in 2012 in which they used fMRI to measure neural signals in response to asthma-specific emotional cues after exposing asthma patients to allergen. These observations allowed them to begin to identify "neurophenotypes" for asthma.
In 2016, they published data from a different approach. Using a type of Positron Emission Tomography (PET) scan that administers a small amount of radioactive tracer to track metabolically active regions of the brain, researchers identified how the brains of asthma patients with high or low levels of chronic stress in their lives responded while experiencing a situation designed to be socially stressful. They also measured airway responses.
Although the study was small - 15 people with high chronic stress and 15 with low chronic stress - both brains and lungs responded differently. Chronically stressed people with asthma appeared primed for enhanced lung inflammation.
Poking the Brain and Probing the Lung
The MINA study, funded by the National Institutes of Health, is considerably larger and more comprehensive than any of the collaborators' prior investigations into this topic. Their goal is to enroll subjects with mild to moderate asthma.
In the first arm of the study, they are investigating the lung-to-brain communication. "We're looking at defining what goes up the immune elevator here, rather than down the elevator," said Dr. Busse jokingly.
First, the team of asthma and pulmonary clinicians will characterize the subjects’ asthma by measuring lung function and analyzing features of airway inflammation following a procedure called segmental bronchoprovocation in which a substance they are allergic to such as ragweed, dust mite, or cat allergen is placed directly into an isolated airway. They also undergo fMRI scans to assess activity in areas of the brain, particularly those which might be responsive to stress.
"The reason we use a segmental challenge [instead of inhaling antigen, which challenges the whole lung] is because it allows us to only interrogate isolated airway segments, get an intense inflammatory response and retrieve the immune cells causing allergic inflammation, but not cause an asthma attack," said Dr. Rosenkranz.
About 48 hours after the allergen bronchoprovocation, when the inflammatory response is at its peak, each volunteer returns for more fMRI testing. While they're in the scanner, volunteers are asked to perform tasks - naming the color of the asthma-related words presented on a screen - that activates specific brain pathways.
"You can think of it as a way to probe the reactivity of these brain regions. In order to see how sensitive something is, you have to poke it," said Dr. Rosenkranz. The regions of the brain, or neurocircuits, can then be evaluated in relation to the development of allergic inflammation.
Scientists also use standard psychological questionnaires to determine levels of chronic life stress and assess presence of depression or anxiety. "We have a rich set of psychological information on these subjects," said Dr. Rosenkranz.
Ultimately, the team hopes to decipher exactly how mind and body connect when people with asthma experience stress, she said. “What is signaling the brain when you have inflammation in the lungs....How does the brain respond, and what are the consequences?"
Connecting the Dots at the Cellular Level
Because study participants also revisit the pulmonary laboratory for another round of collecting cells and lung fluid as well as blood samples, there’s a treasure trove of material to analyze at the cellular and molecular level. Stephane Esnault, PhD (pictured at right), a senior scientist in the Busse laboratory, is conducting a battery of tests including PCR and ELISA assays to quantify how much inflammation is occurring in lung cells and tissue.

The project also involves RNA-seq, a molecular technique to identify which genes are expressed in a sample. “RNA-seq will help us find new molecular pathways involved in this process that we don't know about yet. It's very exploratory,” said Dr. Esnault. Altogether, these components of the study will involve a tremendous amount of number-crunching. “The biostatistician is going to have a lot of work,” laughed Dr. Esnault.
Putting the Pressure On
The second part of the study investigates the opposite process: instead of lung-to-brain communication, what happens during brain-to-lung communication?
To do this, volunteers with mild to moderate asthma undergo a socially stressful laboratory experiment. "It's similar to the level of stress most people experience when making a public speech in front of an unfriendly crowd," said Dr. Rosenkranz.
Then, using FDG-PET (the same procedure used in the smaller 2016 study), scientists identify which regions of the brain lit up metabolically during the experiment. After the stressor and PET scan, participants return to the clinic where the pulmonology group administers a whole-lung challenge and then tracks lung function and gathers samples over the next 24 hours. “This will let us determine if the primed lung inflammation we observed in the 2016 study leads to a more severe response to allergen,” said Dr. Rosenkranz.
It's a rigorous and time-consuming process for volunteers. "This study was more involved than the others I have done," said Erin Eagen, a study volunteer. "[It involved] longer appointments and pretty stressful situations i.e. the 'stress test' before the PET scans, having to do an awkward and nerve-wracking stress test during the PET scan, and many questionnaires. The scans themselves weren't a big deal at all. They were actually kind of relaxing."
She found the three bronchoscopies to be "not a very pleasant experience....but they go by very quickly, and then you get to chill for an hour or so and sleep it off or just relax."
Eagen, whose asthma is induced by seasonal allergies, felt that participating in the study was important and worthwhile. "Everyone at UW takes such great care of you," she said. "Never at any time did I feel overwhelmed or unsafe. If you're uncomfortable with any aspect, you can stop at any time. But I was never close to feeling that way." Volunteers are also reimbursed for their time for each study visit.
The MINA study is a large endeavor involving dozens of research personnel and relies on a successful recruitment of volunteers. To find out information about participating, click here.
Dr. Rosenkranz is confident that the effort will yield valuable data and will provide new and meaningful information that will give important insight into the mind-lung connection in asthma.
Toward New Therapies
"My greatest hope for this study is that our knowledge about the way that the brain and immune system interact in asthma is refined so that we can start tweaking how we treat the disease, and offer different and better treatment modalities," said Dr. Rosenkranz.
Dr. Busse agrees. As a physician, if he had better information about immune responses in the lung and how they affect the brain, "...I might treat an asthma patient differently. If I can figure out the mediators that are causing the responses in the brain, I would consider using medications that block this response, or evaluate other methods to modify these responses, such as mindfulness training, for example."
Other examples of "brain-informed asthma treatment" could, for example, include meditation training designed to help people with asthma better manage chronic stress to re-train the brain and immune system in a way that reduces lung inflammation.
“Certain forms of meditation can alter brain circuits that includes those we have found to be associated with inflammation in the lung. We reasoned that meditation might be helpful in reducing symptoms of asthma through its impact on these neural circuits,” said Dr. Davidson.
And it's important for physicians to consider the psychological health of their patients with asthma, explained Dr. Rosenkranz, especially as other studies have shown that suffering from depression or anxiety can decrease the effectiveness of asthma medications. "We want there to be a greater understanding that mental health and physical health are not independent states of being," she said.
For Dr. Busse, it's a culmination of decades of work and a new frontier. "For years, psychological aspects of disease were not appreciated, and the influence of the mind on asthma was often referred to as ‘just being in your head.’ We now appreciate that definite links exist between asthma and activities in the brain. How these linkages work promises new insights into how to more effectively treat asthma."
Resources:
- Busse WW, Kiecolt-Glaser JK, Coe C, Martin RJ, Weiss ST, Parker SR. 1995. NHLBI Workshop summary: Stress and asthma. Am J Respir Crit Care Med 151:249-252.
- Rosenkranz MA, Busse WW, Sheridan JF, Crisafi GM, Davidson RJ. 2012. Are there neurophenotypes for asthma? Functional brain imaging of the interaction between emotion and inflammation in asthma. PLoS One. 7(8):e40921.
- Rosenkranz MA, Esnault S, Christian BT, Crisafi G, Gresham LK, Higgins AT, Moore MN, Moore SM, Weng HY, Salk RH, Busse WW, Davidson RJ. 2016. Mind-body interactions in the regulation of airway inflammation in asthma: A PET study of acute and chronic stress. Brain Behav Immun. 58:18-30.
- Volunteering for the MINA Study