DOM COVID-19 Journal Club: Variation in false-negative rate of reverse transcriptase polymerase chain reaction-based SARS-CoV-2 tests by time since exposure (review of previous studies)
Study objectives: The authors aimed to estimate the false-negative rate of the SARS-CoV-2 RT-PCR by days since infection.
Methods and Results: Data from seven previously published studies on reverse transcriptase polymerase chain reaction (RT-PCR) performance by time since symptom onset were included in a pooled analysis. The studies included a mix on inpatients and outpatients as well as nasopharyngeal, oropharyngeal, and unspecified respiratory samples. If the study reported results from more than one anatomical site, the authors included only results from one site. The researchers then modeled the risk of false-negative RT-PCR results since day 0 (day of exposure) through day 21. Symptom onset was assumed to occur on day 5.
During the four days prior to symptom onset, the probability of a false-negative was high (100% on day 0 decreasing to 68% false-negative on day 4). False-negative results were lowest starting on the first day of symptom onset (day 5, 38%) and continued to decrease until day 8 (20%). Starting day 9, the false-negative rate began to increase again from 21% on day 9 to 66% by day 21. The authors suggest a possible mechanism for the high false-negative rate may be the variability in viral shedding as well as sample collection technique.
Limitations: Major limitations of this study are: (1) It is unclear if those testing negative late in the course of infection (9 days + since exposure) was due to false-negative RT-PCR results or clearance of the infection. 2) There was a great deal of heterogeneity in the types of studies included in the analysis; however, the authors determined this did not have a large impact on the findings as each individual; study was not especially influential. 3) The study was not able to determine if there were differences in false-negative rates between different anatomical sites or by collection technique. 4) The studies included in the analysis only included cases with at least 1 positive RT-PCR result. 5) Lastly, the model used is only able to assess a one-time, known exposure and may not be applicable to individuals with continuous exposure, such as healthcare workers.
Main conclusions: Caution should be used when interpreting RT-PCR tests for SARS-CoV-2, especially when using results for removing isolation precautions or allowing healthcare workers to return to work following exposure. The high false-negative rate may also have implications for contact tracing if a positive patient is misclassified. If clinical suspicion is high and/or the area has a high infection rate, clinical symptoms, epidemiologic evidence, and potentially repeat testing should be used.
References:
- Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in False-Negative Rate of Reverse Transcriptase Polymerase Chain Reaction-Based SARS-CoV-2 Tests by Time Since Exposure. Ann Intern Med. 2020 May 13:M20-1495. doi: 10.7326/M20-1495. Epub ahead of print. PMID: 32422057; PMCID: PMC7240870.
The Department of Medicine COVID-19 Journal Club is dedicated to understanding and applying data on COVID-19 to inform prevention and management efforts for healthcare workers and patients
This article by Ashley Kates, PhD, Postdoctoral trainee, Division of Infectious Disease. Reviewed by Nasia Safdar, MD, PhD, professor, Infectious Disease, vice chair for research, Department of Medicine.
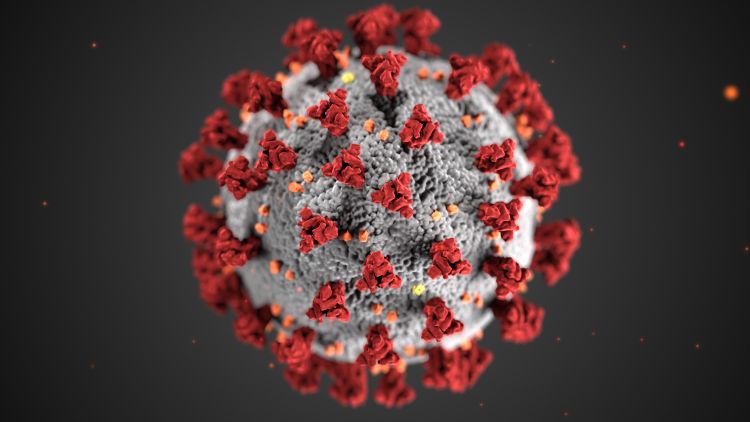
Banner photo: Centers for Disease Control and Prevention image library