DOM COVID-19 Journal Club: Presenting characteristics, comorbidities, and outcomes among 5,700 patients hospitalized with COVID-19 in the New York City area
Study objectives: As limited information is available on patient characteristics and outcomes in the U.S., the authors aimed to describe the demographics, comorbidities, and outcomes of patients admitted to the Northwell Health System, the largest academic medical system, in New York.
Methods and Results: Data was collected via electronic medical record chart review on 5,700 patients hospitalized between March 1st, 2020 and April 4th, 2020. The mean patient age was 63 years (range 0-107), with 60.3% being male and 39.8% being Caucasian. The most common comorbidities upon admission were hypertension (56.6% of patients), obesity (BMI>30, 41.7%), and diabetes (no differentiation between type 1 and type 2 reported, 33.8%). In general, 88% of patients had more than 1 comorbidity. The authors also calculated the Charlson Comorbidity Index – an index used to assess comorbidity burden and 10-year expected survival. The median Charlson Comorbidity index score was 4 (2-6) corresponding with a 53%, corresponding to a 53% estimated 10-year survival.
Upon arrival, 30.7% of patients were febrile and 27.8% required supplemental oxygen. Average temperature was 37.5°C. Other notable vital upon admission were: heart rate over 100 bpm (43.1%), respiratory rate >24 breathes/minute (17.3%), oxygen saturation <90% (20.4%). The first COVID-19 test administered was positive in 96.8% of patients. Second tests were done for previously negative patients if the physician suspected a false-negative or if there were suspected collection errors. Second tests were conducted in 183 patients with 3.2% retesting COVID-19 positive. Co-infections with other viral respiratory pathogens was rare at 2.1%.
3,066 patients remained hospitalized as of April 4th, 2020 leaving 2,634 patients with outcome data. Of these 2,634 patients, 14.2% received ICU care, 22.2% suffered acute kidney injury, and 12.2% required mechanical ventilation. The mortality rate for patients <20 years was 0%. For all other age intervals, mortality rates among males was higher than females. 553 of the 2,634 (21%) of discharged patients died. Mortality rates for those not receiving mechanical ventilation was 19.8% for those 18-65 and 26.6% for those over 65. The average length of stay was 4.1 days with a post-discharge follow-up of 4.4 days. 45 patients required readmission (2.2%) during the study period with a median time to readmission of 3 days. Additionally, diabetic patients were more likely to develop acute kidney injury compared to nondiabetics. Lastly, 7.8% of discharged or deceased patients were taking an ACE inhibitor upon admission and 11.1% were on an angiotensin II receptor inhibitor (ARB). Mortality rates for those on an ACE inhibitor was 32.7% and 30.6% for those on an ARB.
Mechanical ventilation was required for 1,151 patients and at the end of the study period, only 3.3% had been discharged alive with 24.5% deceased, and the remaining 72.2% still hospitalized. Excluding those still hospitalized, 88.1% of patients receiving mechanical ventilation died. Of the patients who died, those with diabetes were more likely to have received mechanical ventilation and/or ICU care. Conversely, those with hypertension were less likely to require mechanical ventilation of ICU care compared to those without hypertension.
Limitations: There are several limitations to this study: 1) The population only included patients from a metropolitan area. 2) The median follow-up time was short at only 4.4 days and may not be able to capture the true outcomes of all patients. 3) No statistical testing or adjustment for confounders was done. 4) Many patients remained hospitalized at the end of the study period and as such, outcome data was only available for 46.2% of patients. As many patients did not have outcome data, mortality rates, especially those associated with mechanical ventilation, may be biased.
Main conclusions: For patients who were either discharged or died: the main comorbidities were diabetes, obesity, and hypertension. Mechanical ventilation was required in 12.2% of patients. 21% of patients died.
Reference:
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Consortium at NC-R. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020 Apr 22.
The Department of Medicine COVID-19 Journal Club is dedicated to understanding and applying data on COVID-19 to inform prevention and management efforts for healthcare workers and patients
This article by Ashley Kates, PhD, research associate, Division of Infectious Disease. Reviewed by Nasia Safdar, MD, PhD, professor, Infectious Disease, vice chair for research, Department of Medicine.
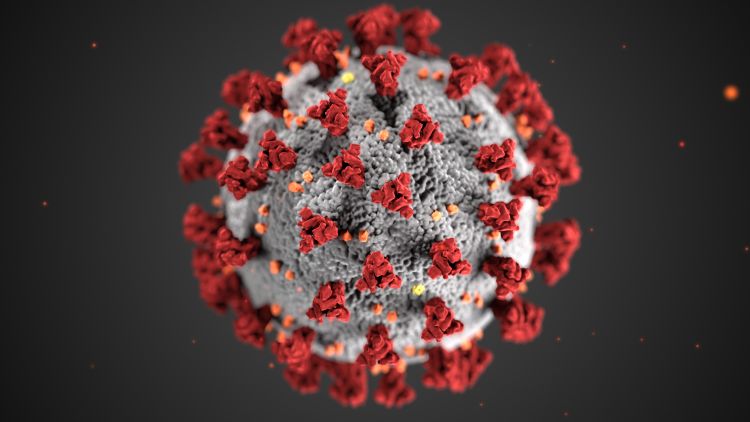
Banner image: Centers for Disease Control and Prevention image library