Study shows impact of multidisciplinary teamwork for hepatocellular carcinoma
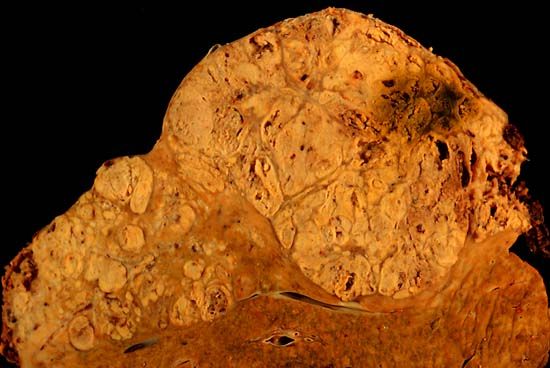


Photo caption: A section from a formalin-fixed specimen taken from an individual who died shows hepatocellular carcinoma occupying much of the volume of a cirrhotic liver. (Public domain image)
Hepatocellular carcinoma (HCC), a form of liver cancer that is the third leading cause of cancer deaths worldwide, is surging in the United States. Cases have tripled in the last two decades, occurring primarily among people age 50. The spike is largely due to hepatitis C viral infections acquired decades prior.
Until recently, HCC had been universally fatal, with a 5-year survival rate of less than 10 percent. Newly available treatments have caused an impressive reversal, with 5-year survival rates now topping 70 percent and most cases of HCC being curable-if caught early enough.
However, wide variation in clinical management of HCC is leading to uneven outcomes. To identify best practices, clinical researchers from the UW-Madison Division of Gastroenterology and Hepatology in the Department of Medicine joined with colleagues from the UW-Madison Departments of Surgery and Radiology, respectively. Their analysis was published in the Journal of Clinical Gastroenterology.
"Our main question was whether having a multidisciplinary team of clinicians caring for HCC patients would provide better results for patients," explained lead author Parul Agarwal, MD (pictured at upper right), assistant professor (CHS), Gastroenterology and Hepatology.
Treating HCC is complicated because it arises in context of underlying liver disease, and there is an increasing array of treatment modalities and regimens to consider. In light of this, many healthcare systems have begun to establish hepatobiliary multidisciplinary tumor boards (MDTBs): a group of clinical professionals from a range of disciplines who meet on a regular basis to review patients referred to the board. Such MDTBs often include hepatologists, medical oncologists, radiologists, surgeons, and pathologists. Tumor board approaches have become common for many other types of cancer, but the use of this team-based approach toward HCC has not been universally adopted. A study published in 2011 indicated that among Medicare beneficiaries with HCC, less than half with early-stage tumors received therapy, and multidisciplinary management was not the norm.
In 2007, UW Health established a hepatobiliary MDTB focusing on liver and pancreas oncology patients. This group of transplant hepatologists, medical oncologists, hepatobiliary and transplant surgeons, pathologists, diagnostic and interventional radiologists meets weekly to consider individual cases referred to the board. After reviewing records and imaging studies, the board makes individualized recommendations. Potential therapies offered may include surgical resection, liver transplantation, thermal ablation, intra-arterial therapies (e.g., chemoembolization and/or radioembolization), systemic chemotherapy, stereotactic radiation, and palliative care.
Would such an approach affect HCC patient outcomes? To find out, Dr. Agarwal and colleagues compared 306 patients with HCC were managed through the MDTB between 2007 to 2011 with 349 patients who were not. All were within the same healthcare system and the groups had comparable demographics in terms of age, sex, and Model of End-stage Liver Disease (MELD) score, which is used to estimate relative disease severity and likely survival of patients awaiting liver transplantation. Of the latter 349 patients, 60 were treated during the 2007-2011 timeframe but had not been referred to the board by their treating physician, and the remaining 289 had been treated between 2002-2007 prior to establishment of the MDTB.
The results were striking: patients in the MDTB group had overall greater survival by nearly 1 year (11.5 months) compared to the non-MBTB group. The MDTB cohort experienced a greater rate of treatment for HCC (odds ratio 2.80), and the type of treatments differed. Patients in the MDTP group had higher rates of thermal ablation (37 percent versus 13 percent), radioembolism (15 percent versus 2 percent), multimodal treatment, and transplantation (24 percent versus 14 percent). The analysis showed that MDTB involvement in HCC care independently predicted survival - even when patients were stratified based on tumor stage at presentation.
"We think the main take-home message of this study is that improved communication within the matrix of professionals involved in the care of HCC patients has a tremendous impact," said Dr. Agarwal. "Higher levels of more effective care improved survival. This indicates that a multidisciplinary approach to coordinate, individualize and optimize care of people with HCC is imperative."
The work gave strong support to the adage that 'more heads are better than one' with regard to clinical management of HCC. "This study, which provided an excellent training opportunity by including residents and fellows in the analysis effort, highlights the value of collaborative clinical work. It shows a combined team at work involving three departments to improve patient care," said Michael Lucey, MD (pictured at lower right), professor and head, Gastroenterology and Hepatology and co-author of the study.
Resources:
- Agarwal PD, Phillips P, Hillman L, Lucey MR, Lee F, Mezrich JD, Said A. 2017. Multidisciplinary Management of Hepatocellular Carcinoma Improves Access to Therapy and Patient Survival. J Clin Gastroenterol. 51(9):845-849.