DOM COVID-19 Journal Club: Studies suggest contradictory evidence on the use of cloth and surgical masks to prevent spread of COVID-19
Prompted by evidence of COVID-19 transmission from asymptomatic individuals, the CDC now recommends that community members wear face coverings such as cloth masks in public. In addition, surgical masks are commonly worn to prevent source spread and have proven effective when worn by patients with influenza in the healthcare setting.
In regards to COVID-19 specifically, the efficacy of surgical and cloth masks in preventing environmental contamination has not been established. To this end, two studies have been recently published that suggests conflicting results on the efficacy of these types of masks.
In the first study, published in Nature Medicine, researchers in Hong Kong collected respiratory and aerosol particles from patients with seasonal coronavirus (n = 17) during 30 minutes of breath [1]. Patients were randomized to wear no mask or a surgical mask. Without a surgical mask, coronavirus was detected in 30% of respiratory droplets and 40% of aerosols. With a surgical mask, coronavirus was not detected in either respiratory droplets or aerosols, suggesting that surgical masks may be effective in preventing the spread of COVID-19. However, this study did not test patients specifically with COVID-19, and the extent to which results can be generalized to that population is unclear [2].
Conversely, a brief research report in the Annals of Internal Medicine presented evidence that surgical and cloth masks worn by four South Korean patients with COVID-19 were insufficient in preventing viral contamination to the environment [3]. The patients included 2 men and 2 women, ranged from 35 to 82 years old, and were hospitalized with pneumonia or upper respiratory infections. Virus was collected from a petri dish held 20 cm from the patient’s mouth during 5 coughs in the following sequence: no mask, surgical mask, cloth mask (2 layers of 100% cotton), and again with no mask. The median viral loads collected without a mask, with a surgical mask and with a cotton mask were 2.56, 2.42, and 1.85 log copies/mL respectively, suggesting a possible reduction wearing a cloth mask. Importantly virus transmission was not not examined in this study. Additionally, they reported contamination on the outside of the mask that may be due to air leaking around the masks.
This brief report has several limitations and should be interpreted with caution. The sample size of four patients is notably small. Mask fit is likely an important factor in effectiveness, but no information regarding mask fit in the study was reported. The effect that the masks had on the projection of particles beyond 20 cm was not evaluated, making it possible that the masks may yet be beneficial at distances that are more often encountered in social interactions and if the healthcare worker is wearing a mask. Lastly, this study was performed in symptomatic patients and it is unknown if these results generalize to preventing COVID-19 spread by asymptomatic individuals.
Taken together, these studies offer initial evidence indicating that there is value in examining the relative effectiveness of different types of masks in prevention of droplet and aerosol in the environment. However, given that virus transmission was a not a feature of either study, these are not considered to be practice changing. Importantly, surgical and cloth masks could introduce contamination to hands by touching the outside of the masks and give a false sense of security. Continuing heightened use of measures such as additional barriers, distancing, and hand-washing will remain vital to preventing COVID-19 transmission.
References
- Leung, NHL, et al. Respiratory virus shedding in exhaled breath and efficacy of face masks. Nature Medicine, 2020.
- Wölfel R, et al. Virological assessment of hospitalized patients with COVID-2019. Nature, 2020.
- Bae S et al. Effectiveness of Surgical and Cotton Masks in Blocking SARS–CoV-2: A Controlled Comparison in 4 Patients. Annals of Internal Medicine, 2020.
The Department of Medicine COVID-19 Journal Club is dedicated to understanding and applying data on COVID-19 to inform prevention and management efforts for healthcare workers and patients.
This article by Alex Birdsill, PhD, research associate, Geriatrics, and neuropsychology fellow, Department of Neurology. Reviewed by Nasia Safdar, MD, PhD, professor, Infectious Disease, vice chair for research, Department of Medicine.
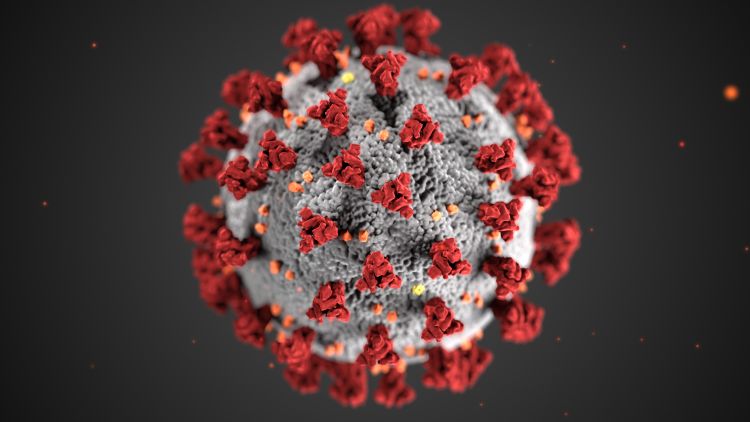
Banner image: Centers for Disease Control and Prevention image library