DOM COVID-19 Journal Club: Pilot study suggests trials of convalescent plasma therapy for COVID-19 are feasible
Convalescent plasma (CP) therapy involves transfusing neutralizing antibodies from recently recovered patients to aid current patients. Previous research has suggested that CP therapy is safe and reduces mortality in SARS, MERS, and H1N1.1-3 However, these previous studies have been small and often lacked control groups. Further, a trial of CP therapy for Ebola virus did not show a reduction in mortality.4 Currently, there are no agents with established efficacy for treating COVID-19, raising great interest in the use of CP therapy. A recent publication in the Proceedings of the National Academy of Sciences (PNAS) reported a pilot study investigating CP therapy for COVID-19.5 The primary endpoint of the study was safety of CP transfusion and the secondary endpoints were clinical, laboratory, and radiological improvements within 3 days of CP transfusion.
The study sample included ten COVID-19 patients hospitalized in Wuhan, China, who received a single 200-mL CP transfusion. The sample included six men and four women, the median age was 52.9 years, and the median time from symptom onset to CP transfusion was 16.5 days. At the time of transfusion, all were considered severe based on one of the following: 1) respiratory distress (RR ≥30 beats/min); 2) oxygen saturation level less than 93% in resting state; or 3) partial pressure of oxygen (PaO2)/oxygen concentration (FiO2) ≤ 300 mmHg (1 mmHg = 0.133 kPa). Ten donors were recruited who recovered from COVID-19, operationalized as a normal body temperature for more than 3 days, resolution of respiratory tract symptoms, and two negative sputum tests of COVID-19 by RT-PCR assay with a one-day sampling interval. All donors had a neutralizing antibody titer above 1:640.
Regarding safety, an evanescent facial red spot was reported in one patient, but there were no serious adverse events. Results of the secondary endpoints reported clinical symptom improvement in all 10 patients. They noted that most patients were either weaned from ventilation or required less oxygenation. Laboratory tests reported an improvement in markers of inflammation and liver dysfunction (CRP, Lymphocyte, ALT, and AST). Chest CT images taken before and after CP transfusion showed absorption of lung lesions to differing degrees after CP transfusion. The authors observed that patients who received CP before 14 days of illness appeared to have better clinical outcomes.
The study retrospectively selected a control group matched in age, gender, and disease severity to the CP treatment group. While all patients in the CP treatment group were either discharged or improved, the historical control group included three deaths, six cases in stable condition, and one case of improvement. This comparison starkly contrasts the treatment group with the control group, but is severely limited since the study was not randomized. While it was reported that there were no statistically significant differences between the groups at baseline, this is likely a product of the small group sizes and group differences may yet prove to be clinically meaningful. For example, according to supplementary material published with the main article, the median C-reactive protein value was 55.9 mg/L in the treatment group and 96.70 mg/L in the control group. Further, it was not reported how adjunctive treatments compared between the groups. Patients in the treatment group received a number of different antivirals, glucocorticoid therapy, antibiotics, and antifungals in addition to CP and it is unknown if and how any of these agents affected recovery.
In conclusion, this small study demonstrates feasibility for larger randomized studies to investigate the use of CP therapy for COVID-19. Although no serious adverse events were reported in this study of ten patients, monitoring and mitigating potential risks will be important in larger trials. In terms of clinical improvement, the small sample size and lack of randomization precludes making any conclusions, leaving it up to further trials to establish efficacy.
References:
- Ko JH et al. Challenges of convalescent plasma infusion therapy in Middle East respiratory coronavirus infection: a single centre experience. Antivir Ther. 2018;23(7):617-622.
- Hung IF et al. Convalescent plasma treatment reduced mortality in patients with severe pandemic influenza A (H1N1) 2009 virus infection. Clin Infect Dis. 2011;52(4):447-456.
- Mair-Jenkins J et al. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis. J Infect Dis. 2015;211(1):80-90.
- van Griensven J et al. Evaluation of Convalescent Plasma for Ebola Virus Disease in Guinea. New Engl J Med. 2016; 374(1):33-42.
- Duan K et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Nat Acad Sci. 2020;202004168.
The Department of Medicine COVID-19 Journal Club is dedicated to understanding and applying data on COVID-19 to inform prevention and management efforts for healthcare workers and patients.
This article by Alex Birdsill, PhD, research associate, Geriatrics, and neuropsychology fellow, Department of Neurology. Reviewed by Nasia Safdar, MD, PhD, professor, Infectious Disease, vice chair for research, Department of Medicine.
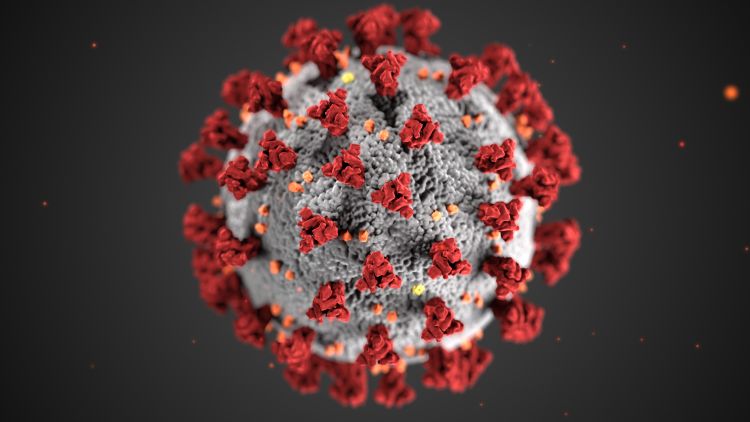
Banner image: Centers for Disease Control and Prevention image library