Cardiovascular advances take center stage at the 2018 American Heart Association Scientific Sessions
Members of the Division of Cardiovascular Medicine were among the 20,000 people attending the 2018 American Heart Association Scientific Sessions on November 10-12, 2018 in Chicago, Illinois. The Badgers contingent left a strong impression, according to James Stein, MD, professor, Cardiovascular Medicine and Robert Turell Professor of Cardiovascular Research.
“Many researchers were excited to learn how to perform our techniques and/or to collaborate with us on their studies,” said Dr. Stein.
His team presented six posters at the conference using novel ultrasound imaging techniques. A seventh poster on renal dysfunction in end-stage heart failure was presented by Ravi Dhingra, MD, MPH, assistant professor (CHS), and internal medicine resident Inga Melvinsdottir, MD.
For the Stein team, it was an opportunity to demonstrate the capability of their new gray scale ultrasound imaging techniques as a “fortune-telling” method for cardiovascular disease (CVD). “The overall theme from our lab is how novel arterial ultrasound imaging techniques can be used to identify risk of future cardiovascular disease events, like heart attacks and strokes, and can be used to identify very early, pre-clinical changes in arteries in response to exercise and immune-modulating interventions,” said Dr. Stein.
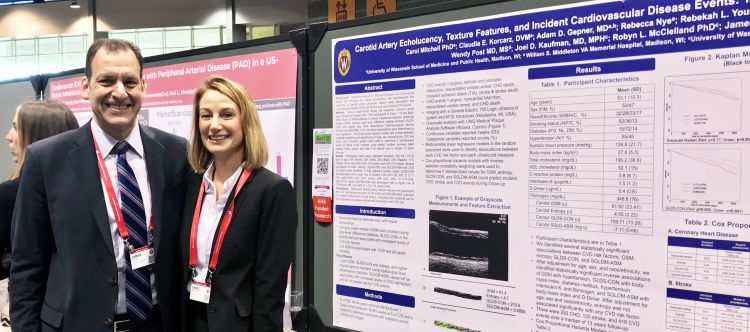
Using image data from the Multi-Ethnic Study of Atherosclerosis (MESA), which involves more than 6,000 men and women from six communities in the United States, the Stein lab showed that gray scale ultrasound measures of carotid wall contrast, entropy, and heterogeneity independently predicted future risk of CVD events.
“This presentation received a great deal of attention from investigators across the world including an invitation to perform our novel analyses – developed and refined by Dr. Carol Mitchell - in a large population-based cohort,” he said.
Adam Gepner, MD, clinical adjunct assistant professor, used a novel speckle-tracking software program to analyze carotid artery ultrasound images from MESA. This allowed him to answer a vexing problem about how the carotid arteries move. “UW already has a substantial reputation in cardiovascular research; I feel that as we continue to present more of our data and grow our research program, our scholarly footprint will continue to expand,” said Dr. Gepner.
The conference highlighted substantial debate within the clinical cardiology community about new clinical guidelines, results from large trials, and research on preventive cardiology. "A lot of new clinical cardiology news came out regarding how to prevent heart disease, including new lipid guidelines and trials showing the benefits of high-dose fish oils in selected patients already on statins, as well as the lack of effectiveness of low-dose fish oils and vitamin D,” said Dr. Stein.
“While all the providers I spoke to are committed to improving cardiovascular health care in the US and beyond, there is still a significant amount of controversy and debate about the best way to go about doing that, specifically as our treatment strategies pertain to newly released guidelines,” said Dr. Gepner.
Much of that interaction is happening via smartphones. “There were a lot more online discussions going on through many social media apps and the AHA scientific session app. This promotes engagement both at AHA and beyond for those who are unable to attend; however, the sheer amount of content and the number of comments and responses can also be overwhelming,” said Dr. Gepner.
“Finding good sources in the infinite pools of ever refreshing content can be difficult, but once you do it can also be an information goldmine for new insights and ideas.”
Members of the Stein group found themselves offering their own insights to other researchers, since their novel gray scale ultrasound approaches offer an advance from traditional linear B-mode measurements of arterial size, thickness, and atherosclerotic plaque count.
Additional applications of the technique included sensitive assessment of vascular changes in patients with virologically-suppressed HIV infection who were randomized to receive methotrexate, an immune suppressant, subtle vascular improvements observed in people with peripheral arterial disease (PAD) who were randomly assigned to a walking exercise regimen, and analysis of the effects of sitosterolemia, a rare, inherited lipid metabolic disorder in members of an Old-Order Amish family in Wisconsin.
Carol Mitchell, PhD, assistant professor (CHS), Cardiovascular Medicine, conducted the HIV study. “Dr. Mitchell demonstrated that low-dose methotrexate led to changes in brachial artery grayscale ultrasound measures like contrast and entropy, indicating possibly favorable effects that correlated with changes in CD4+ and CD8+ T-cell subsets and D-Dimers. These findings were published simultaneously in the AHA journal, ATVB,” said Dr. Stein.
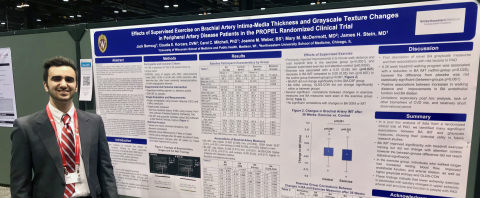 Undergraduate researcher Jack Berroug (pictured at right) conducted the PAD exercise study. “Jack demonstrated that people with peripheral arterial disease randomly assigned to an exercise (walking) regimen, experienced healthful thinning of their brachial artery walls and that improvements in walking distance were associated with salutary changes in arterial wall entropy and contrast. These findings were published simultaneously in Vascular Medicine,” said Dr. Stein.
Undergraduate researcher Jack Berroug (pictured at right) conducted the PAD exercise study. “Jack demonstrated that people with peripheral arterial disease randomly assigned to an exercise (walking) regimen, experienced healthful thinning of their brachial artery walls and that improvements in walking distance were associated with salutary changes in arterial wall entropy and contrast. These findings were published simultaneously in Vascular Medicine,” said Dr. Stein.
And the sitosterolemia study was performed Amy Peterson, MD, associate professor (CHS), Department of Pediatrics. “Dr. Peterson showed how UW can help offer cutting-edge medical care and translate our research tools in to clinical practice in an Old-Order Amish family from Wisconsin that had several members with sitosterolemia. We showed that this disease can have marked phenotypic variability in carotid atherosclerosis burden and physical findings, despite limited environmental and genetic
variability.”
Abstract Titles and Authors:
(presenting author indicated in bold)
- Carotid artery echolucency, texture features, and incident cardiovascular disease events: The multi-ethnic study of atherosclerosis (MESA) by Carol Mitchell, Claudia E. Korcarz, Adam D. Gepner, Rebecca Nye, Rebekah L. Young, Mika Matsuzaki, Wendy S. Post, Joel D. Kaufman, Robyn McClelland, James H. Stein
- Carotid artery displacement and cardiovascular disease risk in the multi-ethnic study of atherosclerosis by Adam David Gepner, Claudia E. Korcarz, Robyn L. McClelland, Rebekah Young, Carol Mitchell, James H. Stein
- Effects of low-dose methotrexate on brachial artery echogenicity and grayscale texture in hiv-infected individuals at increased cardiovascular disease risk: Aids clinical trial group study A5314 by James H. Stein, Eunice Yeh, Joanne M. Weber, Claudia E. Korcarz, Paul M. Ridker, Ahmed Tawakol, Priscilla Y. Hsue, Judith S. Currier, Heather Ribaudo, Carol K.C. Mitchell
- Brachial artery intima-media thickness and grayscale texture changes in peripheral arterial disease patients receiving supervised exercise training in the propel randomized clinical trial by Jack Berroug, Claudia E. Korcarz, Carol K.C. Mitchell, Mary M. McDermott, James H. Stein
- Differential association of various cardiac hemodynamic parameters with renal
Dysfunction in end-stage heart failure patients by Inga Melvinsdottir, Ravi Dhingra - Phenotypic variability in atherosclerosis burden despite genetic and lifestyle homogeneity in an old-order amish family with homozygous sitosterolemia by Amy L. Peterson, James DeLine, Ann M. Dodge, JoAnne Weber, Claudia E. Korcarz, Kristin Hansen, Claire Sandrock, James H. Stein
- The composite inflammatory marker, glyca, and its association with ankle branchial index, carotid plaque and peripheral arterial disease: The multi-ethnic study of atherosclerosis (MESA) by Oluwaseun E. Fashanu, Abayomi Oyenuga, Di Zhao, Martin Tibuakuu, Samia Mora, James D. Otvos, James H. Stein, Erin D. Michos