Innovating Improvements in Internal Medicine
Researchers in the Division of General Internal Medicine lead innovative research that improves health systems, physician well-being and medical education—locally and nationally.
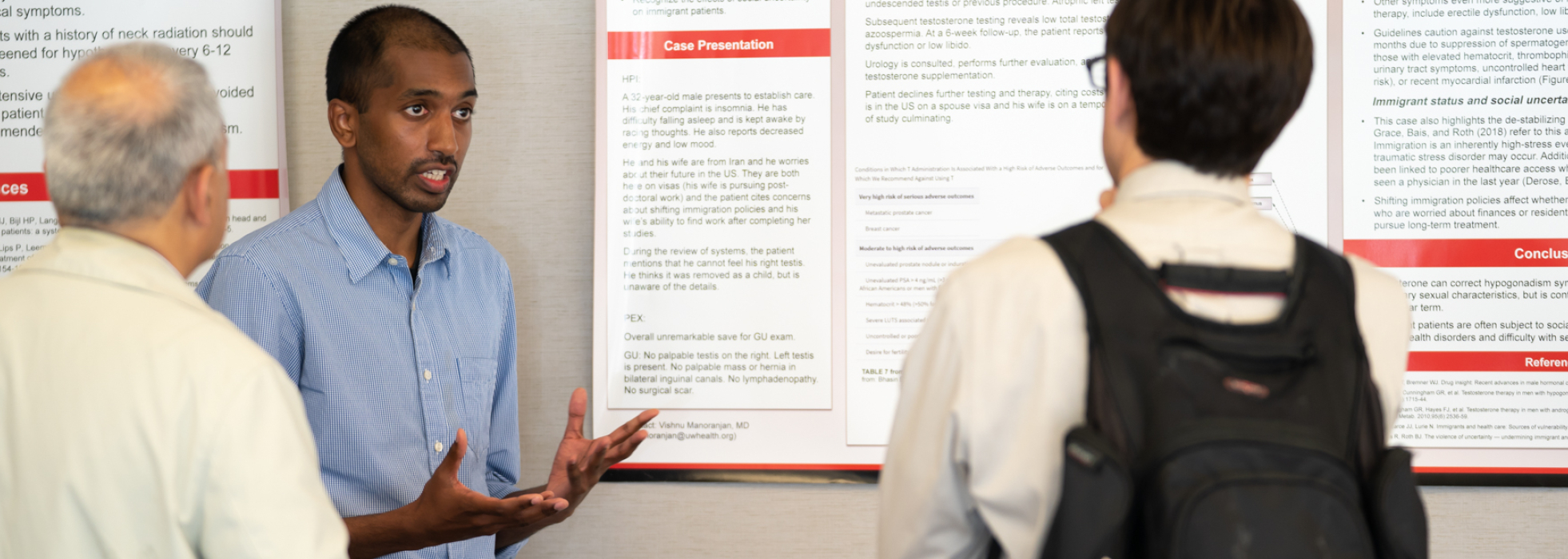
Our division is also home to a GIM Scholars group that presents at an annual showcase and at national conferences, such as the Society for General Internal Medicine.
Our investigators work to transform medicine every day. Get to know them below.
Data Science and Clinical Informatics
Health Services Research
Medical Education and Career Development
Tobacco Use Disorders


Innovate With Us
No matter where you are in your career, our department's robust environment—and our partnerships with the world-class UW-Madison—will help you launch and maintain a successful research program.