DOM COVID-19 Journal Club: Cardiovascular disease, drug therapy and mortality in COVID-19
Purpose: A study to investigate the relationship between underlying cardiovascular disease and COVID-19 outcomes in addition to evaluating the association between cardiovascular drug therapy and mortality in patients with COVID-19.
Study Design: Observational study using de-identified data from the Surgical Outcomes Collaborative international registry from 169 hospitals in Asia, Europe and North America. The database was used to evaluate the relationship of underlying cardiovascular disease (coronary artery disease, heart failure and cardiac arrhythmia) and cardiovascular drug therapy (ACEi/ARB) with in-hospital death among hospitalized patients with PCR confirmed COVID-19 admitted from 12/20/19-03/15/20. Data was controlled for confounders (demographics and co-existing medical conditions). A multivariable logistic-regression analysis was done to examine the effects of age, race, coexisting conditions, hospital location and medications on the likelihood of in-hospital death.
Conclusion: This study confirmed previous observations suggesting that underlying cardiovascular death is associated with an increased risk of in-hospital death among hospitalized COVID-19 (+) patients. Of the 8910 patients with COVID-19, a total of 515 (5.8%) died in the hospital and 8395 survived to discharge. Age >65 (mortality of 10% vs 4.9% among those <65yo; OR 1.93; 95% CI 1.60-2.41), coronary artery disease (10.2% vs 5.2% among those w/o dx; OR 2.70; 95% CI 2.08-3.51), CHF (15.3% vs 5.6% among those w/o HF; OR 2.48; 95% CI, 1.62-3.79), cardiac arrhythmia (11.5% vs 5.6% among those w/o arrhythmia; OR 1.95; 95% CI 1.33-2.86), COPD (14.2% vs 5.6% among those w/o dx; OR 2.96; 95% CI 2.00-4.40) and current smoke status (9.4% vs 5.6% among former or nonsmokers; OR 1.79; 95% CI 1.29-2.47) were all associated with a higher risk of in-hospital death. Non-survivors in this study were older, more often men, likely to be white, had COPD & a h/o smoking with greater prevalence of DM, HLD, CAD, HF and arrhythmias. Factors associated with a better chance of survival to hospital discharge were; female sex, use of ACEi and statins. In summary, COVID-19 (+) individuals with underlying CVD had increased risk of inpatient death but there wasn’t a harmful association with ACEi (2.1% vs 6.1%; OR 0.33; 95% CI 0.20-0.54) /ARBs (6.8% VS 5.7%; OR 1.23; 95% CI 0.87-1.74) drug therapy in COVID (+) individuals with underlying CVD and in-hospital death. ACEi and statins were actually more commonly used by survivors in the study.
Limitation: Confounders can’t be excluded because this wasn’t a randomized controlled trial. There wasn’t a pre-specified primary hypothesis but instead the relationship between several variables were examined for an association with in-hospital death.
Context: The use of ACEi and ARBs were not shown to be associated with in-hospital death of COVID-19 (+) patients with underlying CVD. In clinical practice, these medications should not be discontinued in a COVID-19 patient with underlying CVD in the absence of clinical evidence of harm.
Reference:
- Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19. New Engl J Med. May 1, 2020.
The Department of Medicine COVID-19 Journal Club is dedicated to understand and applying data on COVID-19 to inform prevention and management efforts for healthcare workers and patients
This article by Shenikqua Bouges, MD, advanced fellow, Geriatrics and Gerontology. Reviewed by Nasia Safdar, MD, PhD, professor, Infectious Disease, and vice chair for research, Department of Medicine.
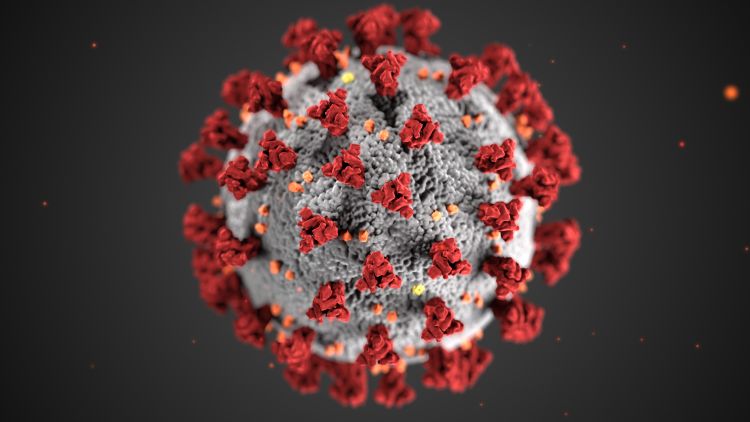
Banner image: Centers for Disease Control and Prevention image library