What is the Coach Program?
The COACH program stands for:
Clarifying learning Outcomes and providing Actionable feedback with Coaching to Help learners succeed
It provides a method for faculty to guide a learner's development by focusing feedback on specific actions and behaviors, next steps for growth and clearly defined outcomes. This will help "coach" a learner through a permanent change in behavior.
Steps to Effective Feedback
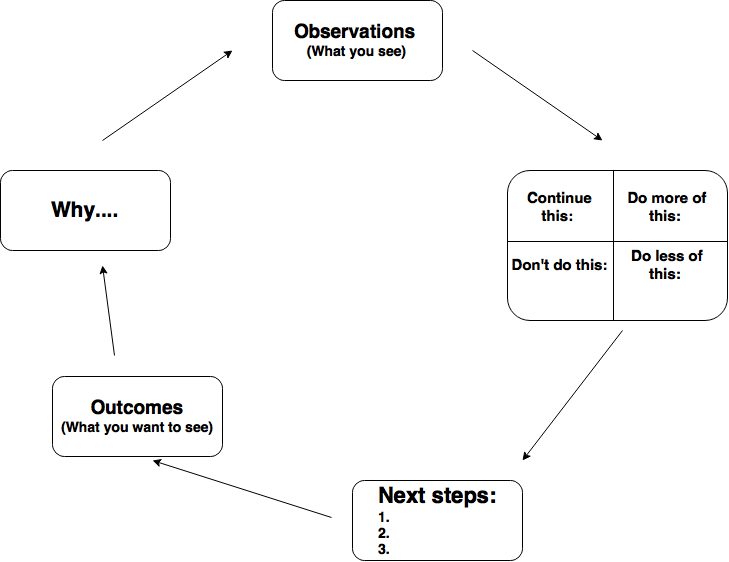
- Observe behaviors and divide into positive feedback and areas for growth
Use the Four box model to provide this feedback:
+ Continue this Do more of this - Do this differently Do less of this
Your “this” should be very specific:
Focus on demonstrated actions and behaviors rather than on the person
Focus on descriptions instead of judgment- Provide next steps as specific directions and tasks for growth, instead of generalities
- Identify the specific outcomes you would like to see as a result of the tasks
- Tell the learner why this is important
Coach Program Methodology
This video discusses the COACH Program methodology for medical students; however, the same strategies are appropriate for other learners, including postgraduate medical trainees.
Examples of Affirmative Comments
The value of affirmative comments for learners is to provide specific, actionable feedback on actions that the learner can continue and expand. Affirmative comments help the learner become aware of areas of emerging strength, and refine their efforts in these areas. Affirmative comments can be inherently encouraging. When provided with actionable information, affirmative comments also illustrate a path for learners that allows them to envision a future state of greater confidence and competence in specific skillsets.
- Information Synthesis
Examples of affirmative comments in the area of information synthesis and/or knowledge synthesis:
- accurately identified diagnoses and plausible alternatives for diagnoses
- identified tests that determine the likely diagnoses
- identified treatments for the likely diagnoses
- accurately identified key features and natural history of the patient's diagnoses
- effectively categorized the differential diagnosis into life threatening vs more likely etiologies
- creates an appropriately broad differential and accurately narrows it based on the clinical data
- consistently and independently developed accurate plans with little prompting
- used a hypothesis driven approach to collecting data from histories and physical exams, and then synthesized that into appropriate plans
- assessments were insightful, well-organized and evidence-based
- read extensively about patients’ diagnoses and as a result, was very well prepared for rounds
- took extra time reading the literature and interviewing the patient which resulted in the student developing an accurate differential diagnosis
- Documentation
Examples of affirmative comments in the area of documentation:
- minimizes extra words and avoids repetition in presentations
- presents key features of the history and physical that define the likely diagnoses
- distilled a patient's complicated case into a succinct presentation
- assessments were accurate and treatment plans reflected this
- assessments were hypothesis driven
- addressed all active problems in written notes
- understood a patient’s complex case and provide a concise, clear written note and oral presentation
- Patient Interaction
Examples of affirmative comments in the area of patient interaction:
- advocated for patients by representing their perspective at rounds and in written documentation
- talked to patients outside of formal rounding times to reassure them, keep them up to date on information and to maintain rapport
- demonstrated excellent rapport with patients by sitting at their bedside during each interaction
- Teamwork
Examples of affirmative comments in the area of teamwork:
- readily assisted the team in seeking additional information about patients
- regularly assisted the interns and residents in daily tasks
- knew and asked about all the patients on the team
- took initiative to look up evidence on patients and brought that back to the team
- consistently looked for opportunities to be useful to the team
- was always willing to step up and fill a role, do a task, or take on new patients
- eager to be challenged every day by asking appropriate questions and jumping right into a new situation to learn
- the team relied on the student for updates on the patients, and this information was accurate and complete
- Professionalism
Examples of affirmative comments in the area of professionalism:
- was always looking for feedback and incorporated this seamlessly into work
- all assigned tasks were completed efficiently and thoroughly
- enthusiastically embraced opportunities to try new things
- was motivated to learn new information about any patient on the team
- consistently calm during interactions with challenging patients
Examples of Constructive Comments
When learners’ progress requires bringing attention to areas for improvement, constructive comments provide meaningful and actionable information about how to improve performance and deepen capabilities. Effective constructive comments describe next steps, specify directions and tasks that will aid growth, and provide explicit outcomes. Importantly, constructive comments focus on descriptions (which provide clear guidance for how to achieve a higher level of skill) rather than judgement (which can elicit a risk-adverse mindset that hinders growth as a learner).
- Improve Knowledge
Beginning Learner
- Read about your patient’s main symptoms to determine discriminating history and physical exam findings that distinguish between potential diagnoses. Show you have accomplished this by including pertinent positives and negatives in your note and presentation.
- Read about the tests and treatments for the diagnoses being considered. Show you know this by including what you read in your assessments and plans.Cite your sources to validate your assessments and plans.
Intermediate or Advanced Learner
- Read national guidelines to learn the areas in which the highest level of evidence is substantiated.
- Learn something to help your patient understand more about her/his illness. For example, read about the expected sequelae of the illness and the outcomes and possible toxicities of treatment. Show that you have accomplished this by being able to explain this to a patient under direct observation.
- Read about the specificity, sensitivity and likelihood ratios of the tests being considered. Show that you know these numbers by suggesting tests with high specificity, sensitivity and good likelihood ratios.
- Substantiate how your diagnosis and plan is supported by what you read. Include the authority and validity of the source (text, guideline, level of evidence, RCT, etc.)
- Apply articles you read to your patient based on inclusion and exclusion criteria, demography, severity of illness and comorbidities of the study patients.
- Improve Presentations
Presenting a New H&P
- Include pertinent positive and negative risk factors (HPI, SH, FH), symptoms (HPI) and signs (exam and labs), and known associated diseases (HPI, PMH) with the goal of leading the listener to your diagnosis. Do not begin your assessment until you have reviewed all the data.
- Begin your assessment with a declarative sentence stating your most likely diagnosis and include data that supports this.
- During the assessment, do not rehash the story and do not bring in new subjective or objective patient data.
- Practice until you know your case well enough that you can do this in less than 5 minutes and be able to look at the listeners while presenting.
- Minimize words and avoid all repetition in your presentation.
Presenting an Update of Ongoing Care (Daily Progress)
- Decide what subjective and objective parameters are being followed to determine if patient is improving
- Start with the main problem or diagnosis.
- Include in your assessment a brief statement about whether this problem has improved or not, and state your evidence for the status.
Requesting a Consultation or Transfer to a Higher Level of Care
- Start with the consult question or defining what you want to see happen.
- State the urgency of the consult.
- Offer a brief background story, summarizing the case in 1-3 sentences.
- Tell the listener how their input will make a difference.
- Improve Assessments and Plans
Beginning Learner
- List all the acute clinical findings from history, physical, lab and radiology. Group findings into likely problems, and then combine problems that are likely of the same origin.
- Look carefully at pertinent positive and negative findings to help rule in/out or increase/reduce the likelihood of diagnoses.
- Decide your most likely diagnosis, alternative diagnoses and not-to-miss diagnoses. Explain how you will discriminate among them and propose tests to find features that define your most likely diagnosis.
- Develop a management plan using diagnostic tests, therapies and patient education.
Intermediate or Advanced Learner
- While inquiring about a problem, ask a set of discriminating questions about one potential diagnosis at a time. Based on the answers, decide whether the likelihood of that diagnosis is high or low.
- Prioritize your differential diagnosis from most to least likely. Show that you have accomplished this by verbally and in writing committing to your best choice for your diagnosis, and by emphasizing the key positive and negative discriminating and defining features in your written notes and oral presentations.
- Focus your more meticulous aspects of your general exam on findings that will further discriminate between the most likely diagnoses.
- Align your diagnostic and treatment with 1) your diagnosis, 2) any alternatives or not-to-miss diagnoses that have not yet been ruled out (and require treatment pending further tests) and 3) with the patient’s and family’s wishes.
- Ask WHY, so that you understand why a patient is on a therapy and HOW, to know how prior diagnoses were confirmed by finding and personally reviewing primary data.
- Take extra time to think about your diagnoses when:
- The patient has life threatening illness, after physiologic stabilization.
- The patient is not getting better.
- The patient remains undiagnosed.
- Confirmation of prior diagnoses is not available.
- Anticipate the natural history of a patient’s disease. By working with the patient, health care team and community, establish a care program to prevent sequelae of the disease and monitor quality of life and progress.
- Become a Junior Attending
Preparation for Attending Rounds
- Be sure you know the patients’ data prior to attending rounds and decide how you would manage them. This allows you to focus on what and how the learners present, rather than trying also learn about the patient.
- Select something to teach the day prior. Try to either demonstrate something at the bedside or teach in the team room something relevant to an active case.
- Plan ahead on what you hope to observe in each learner and have something easily available to record your observations.
- Develop a daily schedule for seeing patients, being with learners, meeting with the interdisciplinary team, charting and reading relevant literature.
Action During Attending Rounds
- Orient your learners with regard to how you would like your time with them to go. Ask them what they want to learn. Ask about their schedules and when the best time for learning would be for them.
- Begin attending rounds with teaching, but change the order if there are unstable patients to discuss.
- Be sure to have them stop other activities while teaching. If they are distracted ask if they prefer to complete service rounds and return to teaching.
- Allow each learner have at least one chance to present a daily update or new patient and refrain from interrupting. Give immediate feedback, be specific and offer or model behavioral changes that would demonstrate improvement.
- Be sure to ask other team learners for insights on the skills of their peers and other health-care team members to help inform your feedback more completely.
- If there are complex improvements needed, either schedule one-on-one time later with the learner or assign a follow up teaching or coaching exercise to a senior learner.
- Do your more detailed rounds in the afternoon and summarize the day for patients and families showing them you care and are in charge by:
- Sitting and using active listening
- Clarifying any mixed messages from multiple providers
- Talking about what is needed to get them home
- Addressing their agenda
- Summarizing the plan
- Consider role modeling these communication and professional skills for students or the senior on the team. After seeing the patient, verbalize to learners what you purposefully communicated.
- Speak personally with consultants when there is lack of clarity or progress in care despite your team’s best efforts.
- Take your team to review radiology and pathology finding and show them the value of establishing relationships with these colleagues.
- Feedback Narratives
The goal of a supervising teacher is to coach a learner through the steps needed to have a permanent change in behavior. A process for change, as adapted from Albert Bandura’s Social Cognitive Theory and Anders Ericsson’s concepts on deliberate practice, are outlined below:
- Awareness: Help the learner see her or his positive attributes and gaps through self-reflection and feedback. Through critical reflection, teaching and coaching, we can help a learner know how current behaviors could evolve into new behaviors that would fill the gaps and enhance what they are already doing very well.
- Motivation: Elicit from the learner what they want to change. Educe from and develop with them an order of priority that best fits their needs. Discuss with them any additional areas you feel they need to change. Evince from them how these changes will benefit their patients, those with whom they work, themselves and their careers.
- Self-Efficacy: Work with the learner to break down the tasks into feasible components needed to achieve their learning objectives. Help the learner categorize the actions to be taken until the learner feels confident in their ability to accomplish the next steps with the prerequisite knowledge, skills, attitudes and behaviors (KSABs) they already have.
- Positive Outcome Expectations: Help the learner see how actions they will take will close the gaps they hope to fill and allow the outcome they hope to accomplish be achieved.
- Deliberate Practice: Help the learner create a plan, focus her or his efforts on performing the tasks with high attentiveness, practice the next steps over and over and use available supervisors/peers and self-reflection to refine and repeat the needed changes until competency is evident in what they consistently do.
Narrative scripts are provided in tables in a downloadable PDF guide. These tables list each of the common gaps learners have and a menu of choices for feedback to help a supervising teacher coach someone toward actionable next steps that are behaviorally based and targeted toward an expected outcome. Consider the following when you author feedback for the learner:
- Do the comments you author provide feedback on a learner’s demonstrated actions, both those that should be continued and those that should be changed?
- Do your comments describe a learner’s next steps for continued growth as a learner, both for their positive and negative attributes?
- Do your comments provide expected outcomes for recommended next steps?
- Is your feedback specifically instructive, descriptive, timely, selective and behaviorally based as opposed to general, inferential, delayed, overwhelming and judgmental?